

Pancreatic cancer starts in the pancreas , an organ located behind the stomach that helps with digestion and blood sugar regulation. The majority of pancreatic cancers begin in the exocrine cells , which produce digestive enzymes, and are called adenocarcinomas .
There are two main types:
The following factors may increase your risk of developing pancreatic cancer:
Pancreatic cancer is often diagnosed at later stages because early symptoms can be vague. Symptoms may include:
If you experience persistent symptoms, it's important to seek medical attention.
Stage I: Cancer is confined to the pancreas.
Stage II: Cancer has spread to nearby lymph nodes or tissues
Stage III: Cancer has spread to major blood vessels and nearby organs
Stage IV: Cancer has spread to distant organs, such as the liver, lungs, or peritoneum
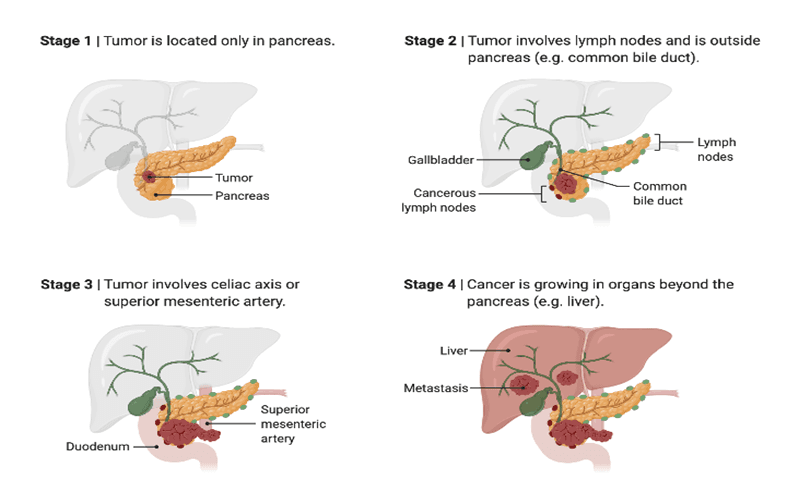
Staging helps determine the best course of treatment.
Treatment depends on the cancer stage, location, and overall health of the patient. Common treatment options include:
Surgery
Surgery is typically only an option for tumours confined to the pancreas and can improve survival chances.
Chemotherapy
Radiation Therapy
It's often combined with chemotherapy or used for patients who can't undergo surgery.
Targeted Therapy
Immunotherapy
Palliative Care
While there's no guaranteed way to prevent pancreatic cancer, lifestyle changes may reduce the risk:
PAC-MANN Blood Test: Researchers at Oregon Health & Science University have developed an inexpensive blood test called PAC-MANN, which detects pancreatic cancer with 85% accuracy, even in its early stages. The test measures changes in protease enzyme activity and costs less than a penny per sample, making it accessible for underserved areas.
AI-Powered Imaging Tools: Northwell Health has introduced an AI-powered tool named iNav, which analyses MRI and CT scans to identify early signs of pancreatic cancer. This proactive approach has reduced the time from diagnosis to treatment by 50%.
KRAS Inhibitors: Pancreatic cancer is characterized by mutations in the KRAS gene. New treatments targeting this mutation, such as daronrasib, have shown promise in early trials, offering extended survival for patients with advanced stages of the disease.
NRG1 Fusion Targeted Therapy: The FDA approved Merus NV's therapy, Bizengri (zenocutuzumab), for treating pancreatic cancers linked to the NRG1 gene fusion. This therapy blocks the interaction between the HER3 protein and the NRG1 gene, inhibiting tumour growth.
High-Dose Vitamin C: A study by the University of Iowa Health Care Carver College of Medicine found that administering 75 grams of vitamin C thrice weekly significantly enhanced the efficacy of chemotherapy for pancreatic cancer patients, doubling overall survival from 8 months to 16 months. .
Irinotecan Liposome-Based Regimen: The FDA approved irinotecan liposome in combination with oxaliplatin, fluorouracil, and leucovorin as a first-line treatment for metastatic pancreatic adenocarcinoma. This regimen has shown improved efficacy compared to traditional treatments.
Irreversible Electroporation (IRE): IRE is a non-thermal ablation technique used to treat locally advanced pancreatic cancer. Clinical data suggest that IRE, when combined with chemotherapy, can improve survival rates and reduce tumour size. However, it remains a high-risk procedure requiring additional safety data before widespread use.
Pancreatic cancer has a poor prognosis, with only about 8.3% of people in England diagnosed between 2016-2020 surviving for five years or more. Survival rates vary significantly by stage; for example, a localized (early-stage) tumour in the US has a 44% five-year survival rate, while a distant (late-stage) tumour has a 3% rate. A major reason for the low survival is the late diagnosis, as symptoms often don't appear until the cancer has grown significantly or spread.
Pancreatic cancer cells feed off hyaluronic acid. Often found in beauty products and wellness supplements, hyaluronic acid attracts and retains water well. It's also a major player in the physiology of pancreatic tumours.
Pancreatic cancer can be present for years without being detected because it often has no early symptoms or causes vague symptoms that are mistaken for other conditions.
While there is no single cause for pancreatic cancer, the main risk factors include smoking, chronic pancreatitis (long-term inflammation of the pancreas, often from alcohol), obesity, and a family history of the disease. Other factors that can increase risk are a diet high in processed meats and fats, developing diabetes, and long-term exposure to certain industrial chemicals.
Pancreatic cancer progression is highly variable, but some studies suggest it can take just over a year for an early-stage (Stage 1) tumor to progress to Stage 4, though the overall development from a pre-cancerous cell to a potentially fatal cancer can take decades.
Pancreatic cancer is most common in middle to older age, with most cases diagnosed in people over 65, and especially in those aged 75 and over.
Yes, alcohol is associated with an increased risk of pancreatic cancer, with the risk growing with higher consumption levels, particularly heavy drinking.
You can search your Pancreatic Cancer Specialist on www.ioncosolutions.com